Background:
Degenerative cervical myelopathy (DCM) is progressive cervical spinal cord dysfunction caused by the narrowing of the spinal canal. [1] Affecting approximately 2.3% of individuals above age 16 [2], DCM is the most common cause of spinal cord dysfunction worldwide [3–5] and classically presents with subjective ataxia, coordination loss, weakness, and sensory changes. [6] There is a need for musculoskeletal therapists such as chiropractors to recognize this condition early in its course [6], as treatment with spinal manipulation may exacerbate symptoms [7, 8], and delayed detection of DCM reduces the likelihood of improvement with surgery. [5, 9]
DCM will become more prevalent as the global population becomes older. [10] While congenital cervical spinal stenosis and smoking are risk factors for DCM, there is a limited understanding of other contributing factors. [3, 11] Diagnostic delay is common, with a mean interval from symptom onset to diagnosis of DCM of 2.2 ± 2.3 years. [12] Providers make the diagnosis clinically as well as by correlating MRI findings of spinal stenosis and electrodiagnostic (e.g., electromyography) results. [11]

Chiropractors are portal-of-entry healthcare providers who commonly manage neuromusculoskeletal complaints, chiefly those of the spine. [13] It is not clear how often chiropractors encounter patients with undiagnosed DCM [14]; however, about 60% of chiropractic patients are at least 55 years old [13], which suggests chiropractors may commonly encounter DCM, given its higher prevalence in older individuals. However, research regarding chiropractic and DCM is limited. In some previous case reports, the chiropractor identified DCM and referred the patient to a surgeon. [15, 16] However, in other cases, the chiropractor did not suspect underlying DCM, which was then aggravated by cervical spinal manipulative therapy [7, 8], a common treatment utilized by chiropractors.
Surgical decompression with or without fusion is the principal treatment used for moderate to severe DCM. [17] While there is limited research regarding non-surgical treatments for DCM, physical therapy, cervical traction, cervical orthoses, spinal injections, and close observation may be appropriate for patients with mild DCM. [18] In one recent prospective study, patients with DCM showed improvements in pain and disability after a program including massage, manual therapies, and exercises. [19] In another case series, patients with cervical canal encroachment, but not acute myelopathy or myelomalacia, showed improvements with cervical spinal manipulation. [20]
Considering little research has examined the management of DCM in the chiropractic setting, and the importance of recognizing DCM to help avoid adverse treatment responses, we present a case in which a chiropractor suspected DCM in a patient and referred her to a spinal surgeon, prompting cervical fusion surgery for severe myelopathy.
Patient Details:
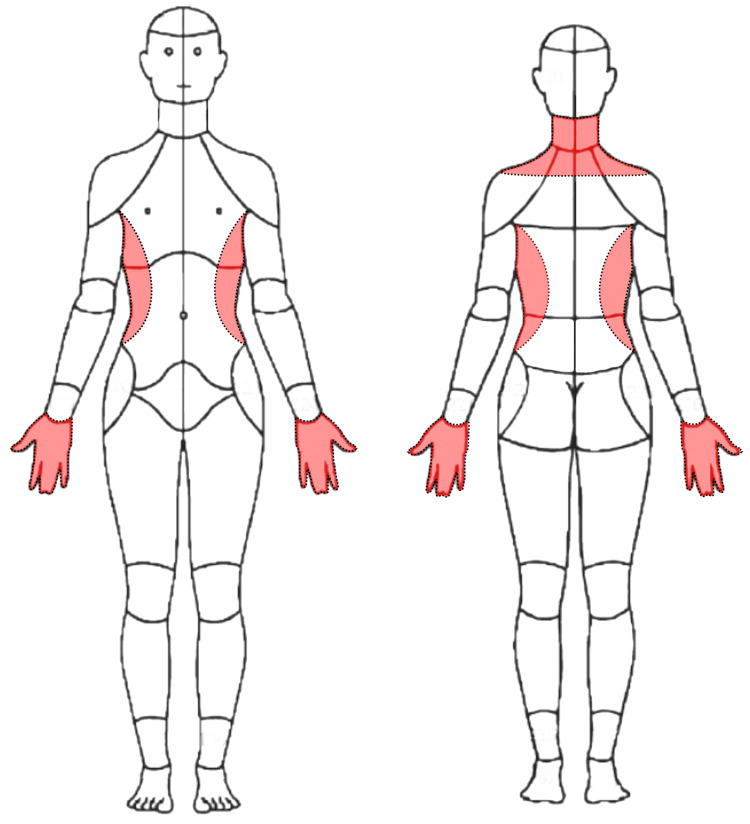
Debbie, a 62–year-old female nonsmoker with a past medical history of asthma, hypertension, and bilateral carpal tunnel syndrome status post bilateral surgical decompression presented to a chiropractor in an integrative setting with a three-month exacerbation of frequent neck pain and tightness, with constant numbness and tingling in her hands diffusely and bilaterally (Figure 1). She rated her current neck pain 3/10 on the numeric rating scale with occasional severe pain at 8/10. She also noted a sensation of warmth along the lateral torso in the region inferior to the axilla extending to the iliac crest (Figure 2). The patient noted that it was hard to hold a pencil and tie her shoes, she dropped things frequently, and had difficulty performing tasks at work due to weakness of her hands. She also reported a reduction in sleep to less than six hours due to her symptoms. She denied any difficulties with walking or bowel or bladder disturbances.
Ten years prior to presentation to the chiropractor, she developed neck pain after she slipped and fell backward on ice. This prompted her to go to the emergency department, where she had radiographs of her cervical spine showing mild degenerative changes at C5–6 and C6–7 (Figure 3). Providers referred her to physical therapy, and according to her physical therapist’s recommendation, she purchased a cervical traction device (Saunders) and used this regularly about a year until her symptoms improved.


Sixteen months prior to presentation she had an episode of moderate-to-severe left neck, shoulder, and arm pain, described as a generalized aching pain, which was keeping her up at night and causing her to become nauseous. She visited her primary care provider, who ordered cervical spine radiographs. These were notable for a grade 1 (i.e., less than 25%) degenerative anterolisthesis of C4 on C5, and multilevel spondylosis (Figure 4). Her primary care provider diagnosed her with cervical radiculopathy and again referred her for physical therapy. The patient also resumed using the cervical traction device at home. The patient reported improvement of her pain with physical therapy, yet noted ongoing numbness and tingling in the right upper extremity. After a brief period of relief, her symptoms fully returned.
Seven months prior to presentation, the patient presented to her primary care provider noting constant neck pain and radiating pain and numbness in the right upper extremity worsened with neck rotation. She noted neck pain that radiated into the right upper extremity when turning her neck to the right side. The primary care provider ordered a cervical spine MRI, the report for which noted moderate spinal canal stenosis from C5 through C7 (Figure 5), severe right foraminal narrowing at C5–6, and severe left neural foraminal narrowing at C6–7. The primary care provider diagnosed the patient with cervical radiculopathy and referred her to pain management.
Two months prior to presentation, the patient saw a pain management specialist who suspected the patient had cervical radiculopathy, secondary fibromyalgia, and had a recurrence of carpal tunnel syndrome. The pain management specialist performed an intramuscular injection of ketorolac tromethamine 60 mg, and later performed a bilateral interlaminar epidural steroid injection at C6–7. This provider also recommended coenzyme Q10 and B-complex vitamins. These therapies did not provide the patient with any relief, and the provider referred the patient to the chiropractor.


Your Task:
Task 1:
Send an email to Dr. Joy providing the summary of the patient’s condition, copy her CA, Maria and ask Maria to pull up the Scan of the patient including other possible documentations that will help Dr Joy’s assessment with the patients condition prior the consultation.
Task 2:
Call Mount Sinai clinic and endorse an MRI request for Debbie, afterward order a monofilament needles 0.25 millimeters (mm) by 40 mm from our official medical supplier.
Task 3:
Book Tina to three chiropractic sessions involving gentle soft tissue manipulation of the upper trapezius and dry needling
Task 4:
Once tasks are done, send an email to the patient and discuss the recurrence of their three chiropractic sessions and dry needling session.
For questions, reach out to: hanna@chiromatchmakers.com
For systems and tools requests, reach out to: help@chiromatchmakers.com

